Voice Sensor Routines Seniors: Meds, Water & Movement (10-Minute Setup)

This guide shows how voice sensor routines seniors can keep meds on time, hydration steady, and movement safe—with a simple setup.
Why Voice Sensor Routines Seniors Improve Daily Habits
Medication adherence for long-term conditions averages ~50% in developed countries; gentle prompts and simple confirmation steps help close the gap. World Health Organization+1
Adults 65+ should aim for 150 minutes/wk of moderate activity + muscle-strengthening + balance work; tiny nudges throughout the day help make this realistic. CDC+1
Good hydration supports healthy aging; typical adequate intakes are ~3.7L/day (men) and 2.7L/day (women) from all fluids/foods (individual needs vary). Mayo Clinic+2National Academies Press+2

The 10-minute starter: voice + sensor basics
🕗 Step 1 — Set three cues
Meds: 8:00 AM and 8:00 PM.
Water: hourly, 9 AM–6 PM.
Move: if no motion for 60–90 min (8 AM–8 PM), nudge to stand/stretch.
🗣️ Step 2 — Create voice routines (Alexa/Google)
“At 8:00 AM, say: ‘Good morning, time for your meds.’ Play a short chime.”
“Every hour 9–6, say: ‘Sip some water.’”
“At 7:30 PM, say: ‘Evening meds reminder.’”
🧭 Step 3 — Add one sensor
Place a hallway motion sensor. If no motion for 60–90 min, flash the lamp and speak: “Let’s stretch for two minutes.”
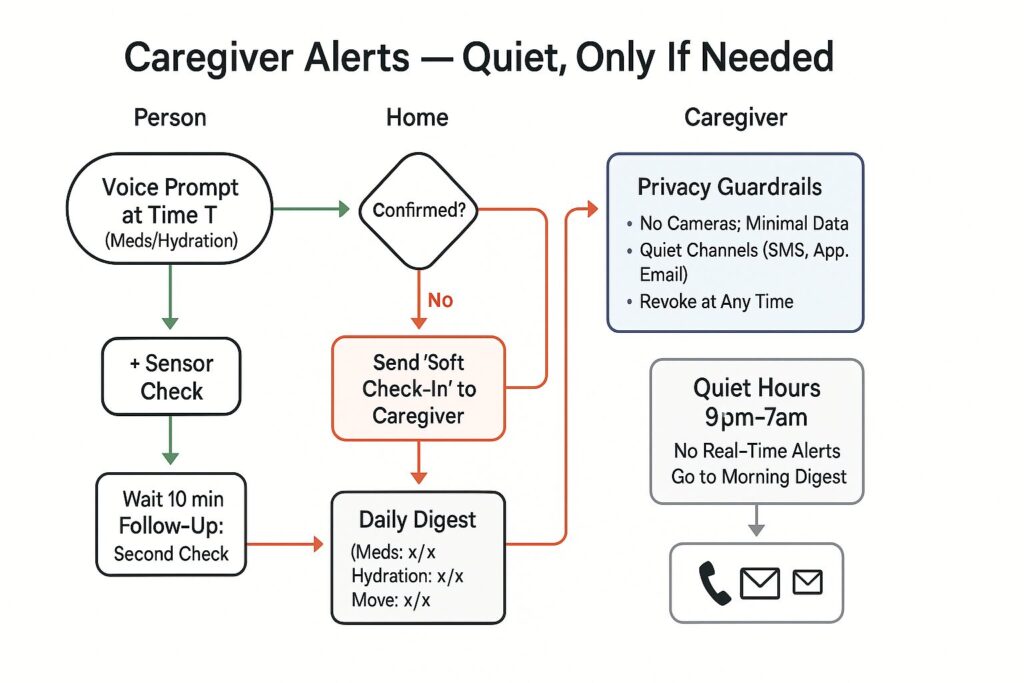
🔁 Step 4 — Build a follow-up
If the user doesn’t say “I took it” or press a bedside button, repeat once after 10 min.
If two attempts fail, send a quiet check-in to Maria (optional).
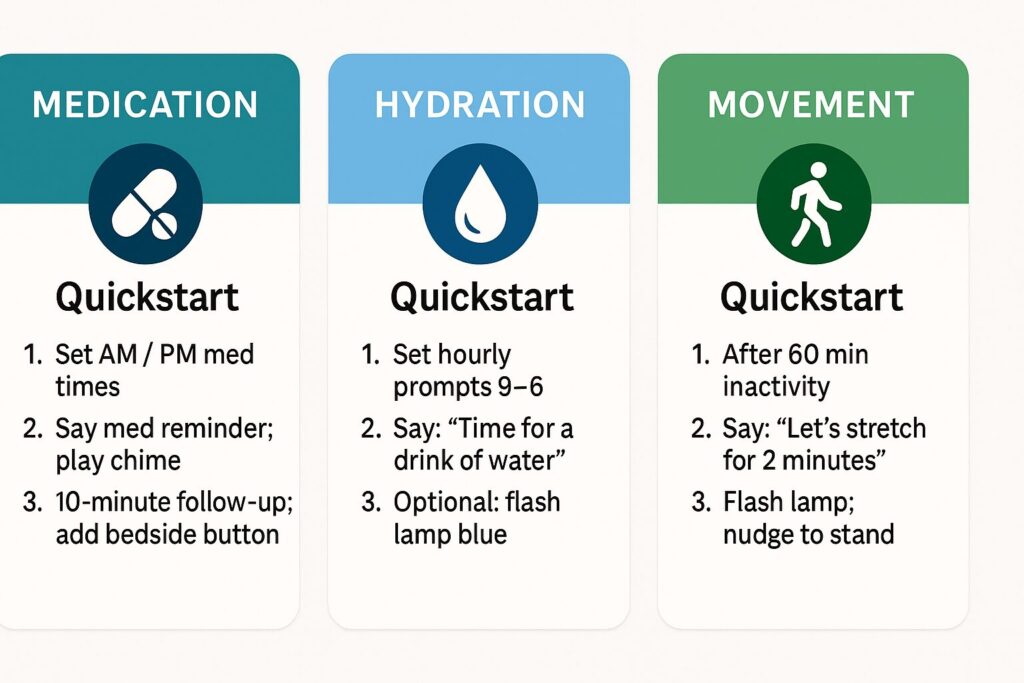
Routine templates (just fill in the times)
💊 Medication (AM/PM)
Trigger: 8:00 AM (repeat at 8:00 PM).
Actions: voice reminder → chime → lamp blue 2 min → follow-up in 10 min if not confirmed.
Optional: contact sensor on pillbox/drawer to detect “not opened by 8:15 AM.”
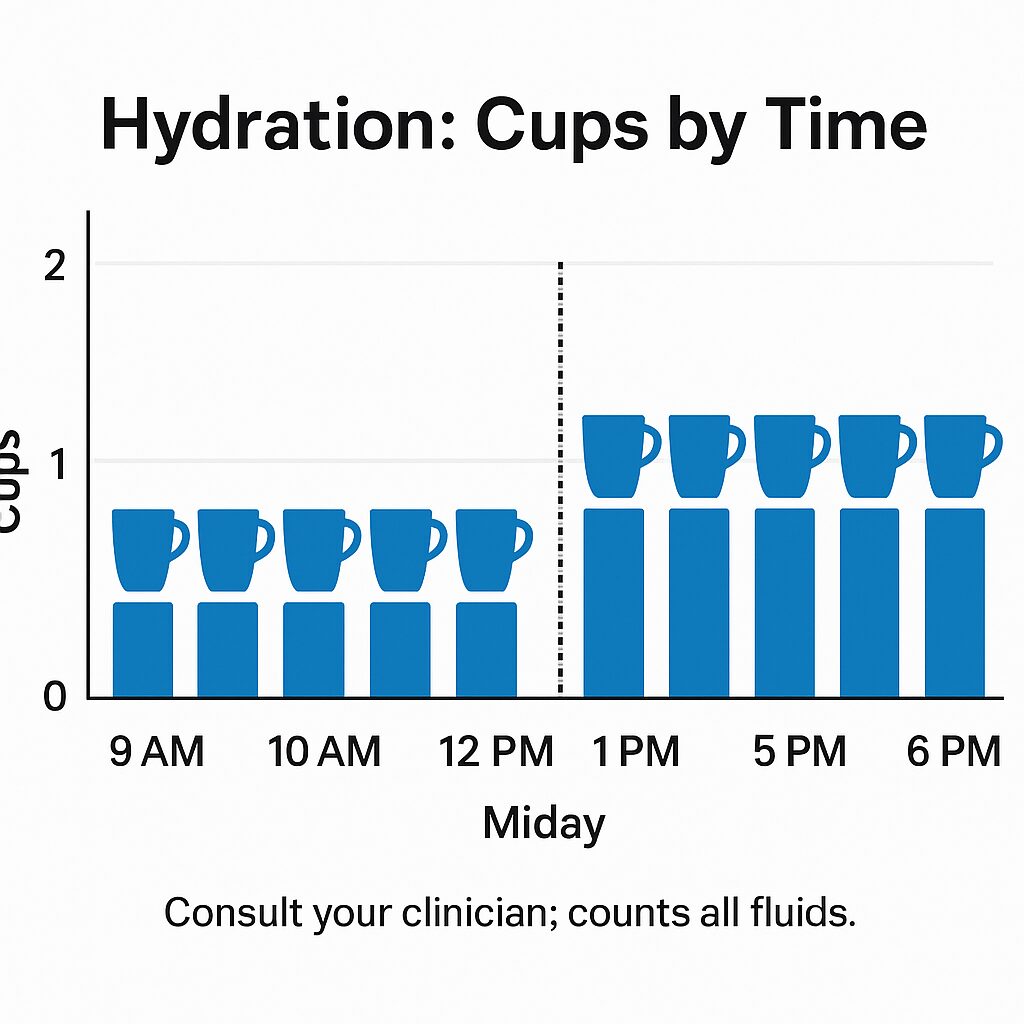
💧 Hydration (hourly)
Trigger: every hour 9–6.
Actions: voice nudge → subtle tone.
Note: counts all fluids/foods; tailor if clinician advises otherwise. Mayo Clinic
🚶 Movement (after inactivity)
Trigger: no motion 60–90 min (daytime).
Actions: voice nudge → lamp flash; suggest 2-minute stretch or hallway lap.
Aligns with strength + balance guidance for older adults. CDC
Sensor options that respect privacy (no cameras)
Motion sensor (hallway): detects long inactivity windows.
Contact sensor (pillbox or medicine cabinet): confirms it opened.
Smart button (nightstand): press to log “Meds taken” or “Hydration done.”
Smart plug/lamp: quick visual blink as a cue.
Persona playbooks: Nancy, Susan, George, Maria
Nancy (independent): start with AM/PM med reminders + one hallway sensor. Add a bedside button to confirm.
Susan (health-focused): after AM meds, voice asks to log BP once daily; email weekly summary to herself.
George (budget-first): begin voice-only (free) + a cheap tally wristband to count water sips.
Maria (caregiver): receive one daily digest (Meds ✅/❌, Hydration prompts, Move nudges). Real-time ping only if two med prompts are missed.
Budget & setup (keep it lean)
Use what you have: a smart speaker and one sensor is enough to start.
Add pieces gradually: button → pillbox contact sensor → lamp flash.
Prefer local routines when possible; share summaries externally.
Privacy & safety notes
Choose no-camera solutions for routine tracking; keep data minimal.
Use Quiet Hours (e.g., 9 pm–7 am) so alerts roll into the morning digest.
Medical needs vary. Check with a clinician for meds, hydration targets, and mobility limits.
Quick checklist (print/save)
☐ Create AM/PM med routines
☐ Hourly water routine (9–6)
☐ Add hallway motion sensor nudge
☐ Add bedside “Done” button
☐ Turn on daily digest (optional)
☐ Set Quiet Hours
FAQ: hydration, activity, and alerts
How much should I drink?
Typical adequate intake is ~3.7L/day (men) and 2.7L/day (women) from all fluids/foods, but individual needs vary; some conditions require limits—ask your clinician. Mayo Clinic+1
How much activity is “enough”?
Aim for 150 min/wk moderate activity, 2+ days of muscle-strengthening, and balance work (e.g., heel-to-toe, chair stands). CDC
Why all the follow-ups?
Because adherence to long-term therapies averages about 50%—gentle repetition helps without nagging. World Health Organization
Citations
CDC — Older Adults: Guidelines (150 min/wk + strength + balance). CDC+1
WHO / “Adherence to Long-Term Therapies.” Global evidence and ~50% adherence stat. World Health Organization+1
National Academies / Adequate Intake for Total Water (3.7L men, 2.7L women); summary via Mayo Clinic & NAP. Mayo Clinic+1
NIH/NHLBI & NIH Research Matters — hydration linked to healthy aging. NHLBI, NIH+1
CDC/NCHS Data Brief — older adults often under-consume relative to AI. CDC
